Pressure Ulcer Prevention in Prone Patients
The prone position has become an increasingly familiar position in the care for patients in critical care.
In fact, there is significant documentation of the benefits of proning patients with acute respiratory distress syndrome (ARDS). As a meta-analysis concluded, when patients are in the prone position for 12 hours or more per day, the mortality rate is reduced.1
Additionally, the positive outcome that critical care clinicians have reported internationally has led to the inclusion of proning as a recommendation in international guidelines for the management of COVID-19.2
In short, proning critical care patients with respiratory compromise can improve oxygenation and lung compliance.3
However, one of the complications associated with proning patients is the increased risk of pressure injuries. A UK-based nationwide survey conducted by the Intensive Care Society (ICS) and Faculty of Intensive Care Medicine (FICM) identified pressure sores as the most cited injury amongst patients positioned in this way. They also identified the need to develop national guidance on managing patients in prone position.4
In response to these findings, the National Stop the Pressure Programme published Pressure Ulcer Prevention Guidance when Nursing Patients in The Prone Position (May 2020). Included in these guidelines are recommendations of skincare and wound care products that can help protect patients’ skin from moisture-associated damage and pressure injuries.
‘It may be helpful to place an absorbent pad with wicking technology under the head so that any oral or nasal fluids, which leak out during proning, are absorbed away from the skin, reducing the length of time the skin is exposed to moisture’.
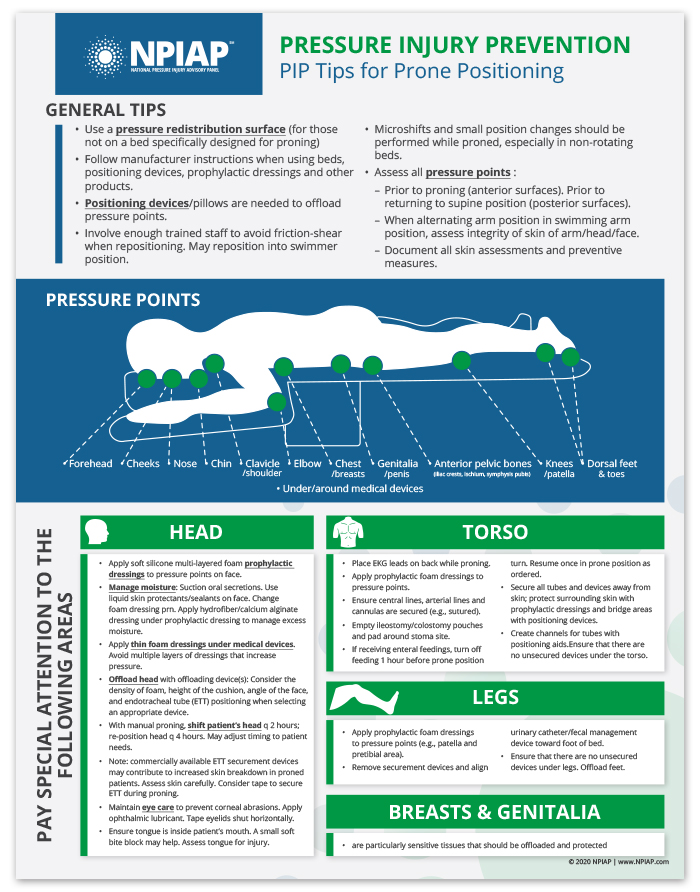
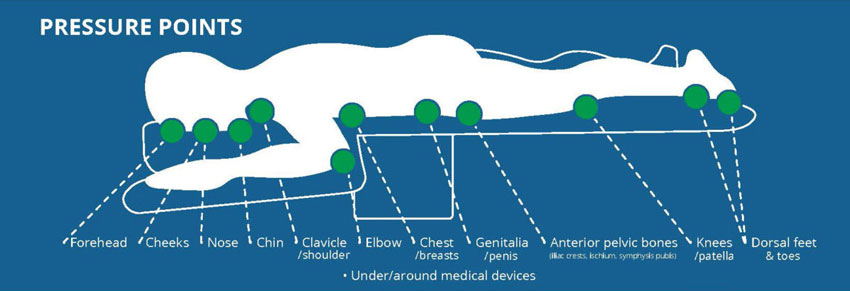
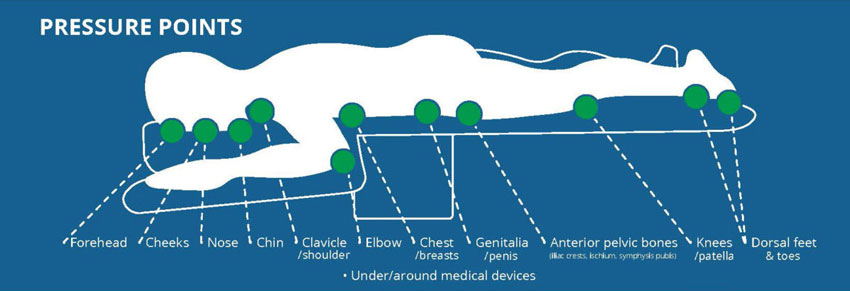
The National Pressure Injury Advisory Panel (NPIAP) indicates areas where prone positioning can increase the risk of pressure injuries.
To help you properly care for patients in the prone position, the NPIAP created a focused three-page document that is downloadable here. It is a visual tool to support clinicians in all aspects of proning patients, including:
- Rationale for proning an ARDS patient
- General guidelines for PIP with prone positioning
- Specific recommendations for the head, legs, torso, and genitalia
- Beds and positioning devices designed to support proning
- Repositioing principles
- Recommendations regarding medical devices
- Swimming position diagram
Key takeaways:
While prone positioning may help treat COVID-19 patients with ARDS, it may also increase their risk of pressure injuries. To help prevent pressure injuries, it is important to follow evidence-based best practice and choose appropriate tools. Remember, this NPIAP resource, now available for download, can help inform your practice and improve skin health outcomes.
Additional resources:
References
1. https://www.atsjournals.org/doi/abs/10.1513/AnnalsATS.201704-343OT (Accessed 15th July 2020)
2. Bamford, P. et al. (2020) ICS Guidance for Prone Positioning of the Conscious COVID Patient 2020 https://emcrit.org/wp-content/uploads/2020/04/2020-04-12-Guidance-for-conscious-proning.pdf (Accessed 21/04/2020)
3. https://www.baccn.org/static/uploads/resources/NRCP_Prone_Position_ICU_pt.pdf (Accessed 10th July 2020)
4. https://emcrit.org/wp-content/uploads/2020/04/2020-04-12-Guidance-for-conscious-proning.pdf (Accessed May 2020)
Related Products