Surgical Site Infection Prevention
There are millions of microorganisms living on the skin, in the body and in the environment. They include bacteria, viruses and fungi. Most of them cause no harm, but in the operating theatre, preventative measures have to be taken to avoid them at all costs.
Microorganisms from the skin or environment can enter the body through the surgical wound during or after the operation. They can multiply and cause an infection known as a surgical site infection (SSI) or a surgical wound infection.1
According to a study done by the NHS in 2015 and 2016, 1,632 out of 136,872 procedures resulted in an SSI.2
In order to avoid SSIs, you have to look for risks factors. In this section, you can find more information on potential risk factors and tips on how to minimise them.
Patient-Specific Risk Factors
Patient-specific risk factors can contribute to SSIs, and while some of these factors can be modified, others cannot.1
The following sections will provide more information about each of these risk factors and potential interventions to minimise these risks.
Age
Elderly patients suffer more from health conditions, illnesses and severe disorders, and they have a decreased immune response to infection.
Furthermore, older patients who develop SSIs have greater morbidity and mortality compared to younger patients.2
Age is not a modifiable factor, so it is important to examine older patients preoperatively. You should define their level of health and identify potential risk factors before the surgery.
Nutritional State
Malnutrition can decrease immune function and contribute to poor wound healing, both of which increase susceptibility to infection.
If a patient is found to be malnourished preoperatively, appropriate interventions should be planned to improve the patient’s nutritional status before the surgery.3
Obesity
Obesity-related immune disorders decrease immune response and can lead to diabetes.
Respiratory and pharmacologic issues related to obesity can also contribute to increased susceptibility to SSIs.4 It is important to assess the body mass index (BMI) of obese patients preoperatively and encourage weight loss and proper nutrition prior to surgery.
Diabetes Mellitus and Hyperglycaemia
Studies have shown that both insulin-dependent and non-insulin-dependent diabetic patients are at an increased risk for developing SSIs.5 This is due to poor immune function and delayed wound healing.
Diabetic patients need to have controlled blood glucose levels preoperatively, intraoperatively and postoperatively. Patients should receive insulin perioperatively to control hyperglycaemia and minimise the risk of adverse outcomes.6
Bacterial Colonisation and Coexisting Infections
Research shows that surgical sites containing more than 100,000 microorganisms per gram of tissue have a significantly greater risk of infection.
However, it is important to note that the number of microorganisms necessary to cause an infection is significantly lower when there is foreign material, such as surgical mesh, at the site.7
If a patient has an existing infection at the time of surgery, this also increases the likelihood of developing an SSI.1
Smoking and Nicotine Use
Smoking reduces oxygen delivery to tissues, damaging wound healing abilities and immune defences.
Quitting cigarettes before the surgery can help increase oxygenation to the tissues, improve healing and reduce the risk of SSIs. Receiving additional oxygen perioperatively can also help improve tissue oxygenation and reduce the SSI risk.8
Immunosuppression
Any medical conditions or medications that cause immunosuppression will increase the risk of SSIs, in particular, steroids that have been linked with postoperative complications.9
References
1 Kirchhoff et al. Patient Safety in Surgery 2010, 4:5 http://www.pssjournal.com/content/4:5 JAMA Surg. 2017;152(8):784-791. doi:10.1001/jamasurg.2017.0904 Published online 3 May 2017. Corrected on 21 June 2017.
2 McGarry S, Engemann J, Schmader K, Sexton DJ, Kaye KS. Surgical Site Infection due to Staphylococcus Aureus in the Elderly: Mortality, Duration of Hospitalization and Cost. Infection Control & Hospital Epidemiology. 2004 Jun; 25(6): 461-467
3 Culebras JM. Malnutrition in the Twenty-First Century: An Epidemic Affecting Surgical Outcome. Surgical Infections. 2013 Jun; 14(3): 237-243
4 Huttunen R, Syrjänen J. Obesity and the Risk and Outcome of Infection. International Journal of Obesity. 2013 May; 37: 333-340
5 Ashar A, Valerian BT, Lee EC, Bestle SL, Elmendorf SL, Stain SC. The Effect of Diabetes Mellitus on Surgical Site Infections after Colorectal and Noncolorectal General Surgical Operations. The American Surgeon. 2010 Jul; 76(7): 697-702
6 Kwon S, Thompson R, Dellinger P, Yanez D, Farrohki E, Flum D. Importance of Perioperative Glycemic Control in General Surgery: A Report from the Surgical Care and Outcomes Assessment Program. Annals of Surgery. 2013 Jan; 257(1): 8-14
7 Monga. M., 2012. Ureteroscopy: Indications, Instrumentation & Technique. Springer Science & Business Media, p.211.
8 Belda FJ, Aguilera L, García de la Asunción J, Alberti J, Vicente R, Ferrándiz L, Rodríguez R, Company R, Sessler DI, Aguilar G, Botello SG, Ortí R; Spanish Reduccion de la Tasa de Infeccion Quirurgica Group. Supplemental Perioperative Oxygen and the Risk of Surgical Wound Infection: A Randomized Controlled Trial. JAMA. 2005 Oct 26;294(16):2035-42. Erratum in: JAMA. 2005 Dec; 294(23):2973.
9 Ismael H, Horst M, Farooq M, Jordon J, Patton JH, Rubinfeld IS. Adverse Effects of Preoperative Steroid Use on Surgical Outcomes. American Journal of Surgery. 2011 Mar; 201(3):305-8
Preoperative Risk Factors
Numerous factors can affect SSI risk before a surgery. The following sections discuss ways to address these risk factors in order to enhance patient safety and improve outcomes.1
Antimicrobial Prophylaxis
If prophylactic antibiotics are needed, they should be administered within one hour before the surgery and stopped within 24 hours afterwards. Continued use of antibiotics to treat a specific infection are the exception to this rule.2
Preoperative Hair Removal
Shaving is ill-suited for this task because it can result in multiple skin abrasions, which can later become infected.2 Hair should only be removed if it is interfering with the operation by using clippers or a depilatory agent.
Preoperative Skin Preparation and Antisepsis
The goal of preoperative skin preparation and antisepsis is to clean the skin and remove microorganisms, reducing the SSI risk.3 The Association of periOperative Registered Nurses (AORN) recommends that patients should shower prior to surgery with either soap or an antiseptic.3
Multidisciplinary teams, including perioperative nurses, physicians and infection prevention specialists, should select safe and effective products for skin antisepsis. The solution used for each patient and each procedure should meet the regulations in place and be appropriate for the patient’s needs in terms of allergies or sensitivities.3
Prior to applying the antiseptic preparation solution to the patient’s skin, the nurse should verify that the skin is free of:
- Soil
- Debris
- Emollients
- Cosmetics
- Alcohol-based products.
Nurses should perform hand hygiene, don sterile gloves and use sterile techniques while applying the skin antiseptic. Once the skin has been prepared, only sterile items should be exposed to the skin.3
Sterile Attire
Personnel in the perioperative area should comply with appropriate guidelines for sterile attire to minimise the patient’s exposure to microorganisms. AORN provides best-practice recommendations for surgical attire:
- Clean surgical attire should be worn in the semi-restricted and restricted areas of the perioperative setting.
- All individuals who enter the semi-restricted and restricted areas should wear disposable scrub attire or scrub attire laundered at a healthcare-accredited laundry facility.
- Personnel entering the semi-restricted and restricted areas should cover their head, hair, ears and facial hair.
References
1 Kirchhoff et al. Patient Safety in Surgery 2010, 4:5 http://www.pssjournal.com/content/4:5 JAMA Surg. 2017;152(8):784-791. doi:10.1001/jamasurg.2017.0904 Published online 3 May 2017. Corrected on 21 June 21 2017
2 Specifications Manual for Joint Commission National Quality Core Measures (2010A1). (2010). Retrieved 23 June 2015 from www.manual.jointcommission.org
3 Conner R (Ed.). Guidelines for Perioperative Practice: 2015 Edition. AORN, Inc. 2015
Intraoperative Risk Factors
The following sections discuss ways to address a variety of intraoperative risk factors.
Surgical Technique
The surgical technique refers to numerous activities performed during the surgery. Surgical technique can vary widely depending on the surgeon and can greatly influence the development of SSIs. Here are a few techniques that can help minimise the risk of infections:
- Achieving adequate haemostasis while simultaneously preserving blood supply to the tissues
- Handling tissues gently
- Avoiding inadvertent perforation of a hollow viscus, such as the stomach
- Removing devitalised tissues that are charred or necrotic
- Properly using drains and suture material and minimising dead space
- Preventing intraoperative hypothermia.1
Foreign Material in the Surgical Site
Foreign materials within the surgical site present a breeding ground for infection.
There is a wide variety of foreign materials, ranging from suture material and surgical mesh to prostheses. They can promote inflammation and bacteria can grow on them.1
Surgical Drains
Surgical drains can potentially increase a patient’s risk of an SSI, particularly if the drains are not handled properly.
When drains are used during a surgery, the likelihood that an SSI will develop is higher. Drains should be placed through a separate incision distant from the surgical incision site.
Additionally, studies have shown that when closed suction drains are used rather than open ones, the incidence of SSI is reduced. The utilisation of drains can be important after the operation and can help effectively evacuate hematomas or seromas.
However, it is important to keep in mind that the timing of drain removal can affect infection rates. Bacterial colonisation of the drain tract will increase the longer the drain is left in place.1
Instrument Sterilisation
Inadequate instrument sterilisation has been associated with SSI outbreaks. It is therefore important to understand the different methods of sterilisation and the guidelines in place in order to ensure the efficacy of the sterilisation process.
There are different methods of sterilisation:
- Steam under pressure
- Dry heat
- Ethylene oxide
- Gamma radiation.1
Perioperative Hypothermia
Many studies have shown that patients who are hypothermic in the perioperative period have increased rates of postoperative complications, including SSIs.
Hypothermia is defined as a core body temperature of less than or equal to 36o Celsius. In the cold operating theatre environment, blood is pushed away from the skin into the core of the body to protect vital organs. This results in decreased perfusion and oxygenation of the skin. Blood vessels in the skin also undergo vasoconstriction, further reducing blood flow.
Furthermore, when the body temperature is low, cellular consumption of oxygen is reduced. This impairs the natural defences within the skin from being able to fight off infectious organisms.3
Adherence to Sterile Technique
The sterile technique process prevents contamination and allows for maintaining a sterile field during procedures. The sterile technique includes:
- Wearing clean scrub attire (including appropriate head and feet coverings)
- Following hand hygiene practices
- Wearing a clean mask for each procedure.
A well-maintained sterile field can influence patient outcomes and reduce infection rates.2
Oxygenation
Adequate oxygen supply to tissues is essential for wound healing and infection prevention. Oxidative killing, or destruction by oxidation, is the most important mode of defence against pathogenic organisms. This process is dependent upon the partial pressure of oxygen in the tissue.4
Operating Theatre Ventilation
The air in the operating theatre may contain dust, lint, skin squames or respiratory droplets, which are laden with microorganisms. The number of microbes in the air is related to the traffic in and out of the operating theatre; therefore, traffic should be limited.
Additionally, operating theatres should maintain positive pressure compared to adjacent areas. This prevents airflow from the adjacent areas, which are presumably less clean, into the operating theatre.1
Length and Type of Operation
Both the length and type of procedure can affect the patient’s risk of developing an SSI.
Longer procedures are associated with a higher SSI risk, and procedures have varying levels of contamination, which directly affect SSI risk.
References
1 Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. American Journal of Infection Control. 1999 Apr; 27(2): 97-132
2 Conner R (Ed.). Guidelines for Perioperative Practice: 2015 Edition. AORN, Inc. 2015
3 Wagner VD. Patient Safety Chiller: Unplanned Perioperative Hypothermia. AORN Journal. Nov 2010; 92(5): 567-571
4 Greif R, Akca O, Horn EP, Kurz A, Sessler DI. Supplemental Perioperative Oxygen to Reduce the Incidence of Surgical-Wound Infection. New England Journal of Medicine. 2000 Jan; 342: 161-167
Postoperative Risk Factors
Risk factors for SSIs are not limited to preoperative and operative causes. Postoperative factors can also affect SSI development.1
Types of Wound Closure
Postoperative wound care can vary greatly depending on the type of wound and how it is closed:
- Primary closure describes fully closing the surgical wound in the operating theatre, with either staples or sutures.
- Secondary closure happens when the wound edges are not initially approximated in the operating theatre. Granulation tissue gradually fills in the wound defect, healing the wound.
- Delayed primary closure happens when the surgical wound is left open following the surgery, but is then closed after a few days of observation if no infection is present.
Both secondary closure and delayed primary closure are used when the wound is thought to be contaminated.2
Incision Care
Wound care depends on the wound and closure type.
Most surgical wounds are closed primarily. These wounds are typically covered with a sterile dressing for 24 to 48 hours. This allows epithelialisation of the wound to occur for protection against infectious external pathogens. After this period, dressings can be quite variable depending on the condition of the wound and if drainage is necessary.
When delayed primary closure or secondary closure techniques are used, the wound is packed with sterile gauze and is then covered with a sterile dressing. As the wound is likely contaminated, it should be left open, as to not trap the bacteria. These wounds should be closely monitored for signs of infection.1
Length of Hospital Stay
An extended hospital stay increases the risk of SSIs.
The longer patients are hospitalised, the more exposure they have to bacteria, particularly antibiotic-resistant bacteria.1
Discharge Planning and Instructions
Patients are often discharged before their wounds have fully healed. Thus, it is important for nurses or other healthcare professionals to give the patient and their family the appropriate wound care instructions. Patients should also be encouraged to contact their surgical team with any questions.1
References
1 Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. American Journal of Infection Control. 1999 Apr; 27(2): 97-132
2 Myers BA. (2008). Wound management principles and practice 2nd ed. Upper Saddle River, NJ: Pearson
Medline Solutions for SSI Prevention
Skin cleaning and disinfection are two necessary steps for the initial reduction of surface bacteria before a surgery. Even though the amount of skin microorganisms is reduced, they are not completely eliminated, and they can survive in microscopic folds of the skin.
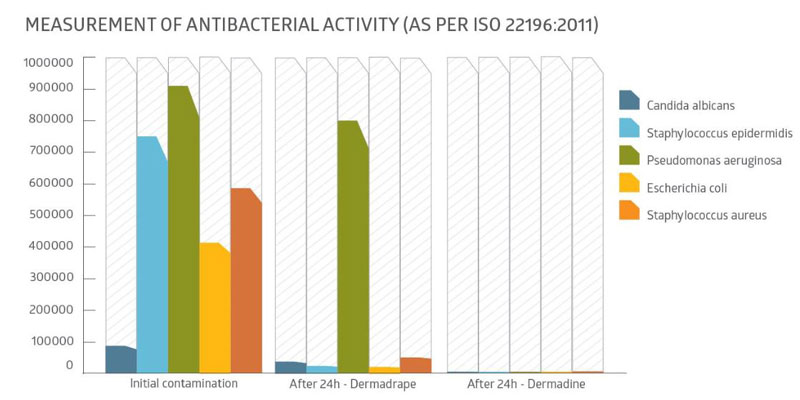
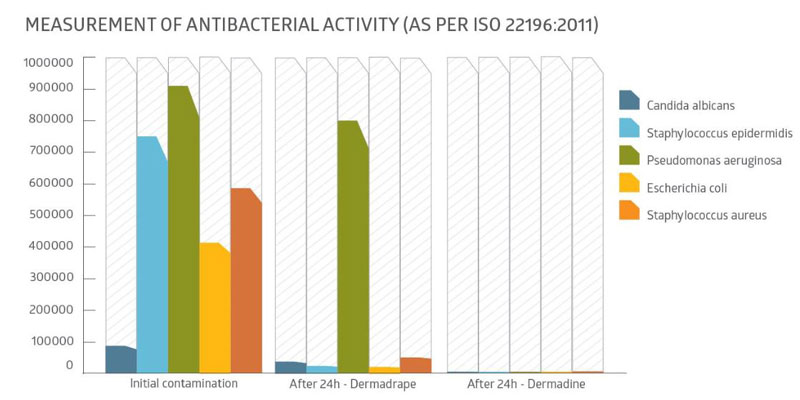
Dermadine Impregnated Incise Drape
When the skin is cleaned and long-lasting asepsis is required, the Dermadine incise drape guarantees that a sterile field is maintained. Its antimicrobial activity against the skin’s microorganisms reduces the risk of SSIs. The Dermadine incise drape provides a constant iodine presence for more than 24 hours, helping reduce the risk of skin flora contaminating the open wound.
Our main product features are:
Fast Acting
When applied, the Dermadine incise drape demonstrates strong antimicrobial activity. Within 30 minutes of application, there is a significant reduction in the bioburden, which is maintained during the surgery.
Conformable and Enveloping
Dermadine is naturally elastic and ultra-thin, ensuring a perfect fit to anatomical structures and joints. It adapts to large muscle deformations (even when autostatic retractors are used) without losing its adhesive properties.
Breathable, Water-Repellent and Waterproof
Dermadine combines blood and water repellence with water vapour breathability to prevent the formation of fluid, which can reduce adhesiveness over the course of the surgery. The breathable film guarantees complete impermeability to microorganisms.
Strong and Anti-Glare
In addition to its resistance to tearing, Dermadine also allows for easy surgical incisions with any scalpel blade and provides the skin indirect protection from tearing. Its anti-glare properties provide perfect visibility at the point of incision under the presence of reflected light.
Adhesion with the Presence of an Antimicrobial Agent
Dermadine’s skin-friendly medical adhesive allows for high-peel adhesion on all areas of the skin, and especially around the wound’s edges, without any irritation. The polyacrylic structure in Dermadine’s adhesive contains an iodophor complex in which a surfactant J-carrier transports iodine and begins releasing it upon application to the skin. The acrylic adhesive is atraumatic during removal, even on elderly patients’ skin, and guarantees no residual adhesive left behind.
Related Products


